ANIMATION
Introduction
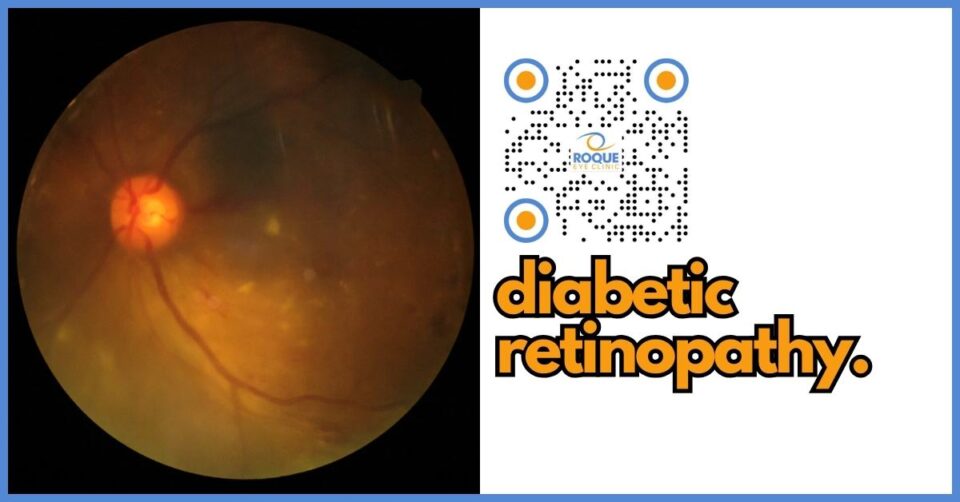
Diabetic retinopathy is a diabetes complication that affects the eyes. It's caused by damage to the blood vessels of the light-sensitive tissue at the back of the eye (retina). Initially, diabetic retinopathy may cause no symptoms or only mild vision problems. However, it can eventually lead to blindness.
The condition can develop in anyone who has type 1 or type 2 diabetes. The longer you have diabetes and the less controlled your blood sugar is, the more likely you are to develop this eye complication.
Key Learning Points
- Understanding Diabetic Retinopathy: Learn what it is, how it affects your vision, and why it occurs.
- Risk Factors: Identify the risk factors associated with diabetic retinopathy.
- Prevention and Management: Explore strategies to prevent and manage diabetic retinopathy.
- Treatment Options: Review the latest treatment options available for managing this condition.
- Patient Empowerment: Gain insights into how you can take an active role in managing your eye health.
What is Diabetic Retinopathy?
The Basics of Diabetic Retinopathy Diabetic retinopathy occurs when high blood sugar levels cause damage to blood vessels in the retina. These blood vessels can swell and leak or close, stopping blood from passing through. Sometimes, new blood vessels grow on the retina. All of these changes can steal your vision.
Stages of Diabetic Retinopathy
- Mild Nonproliferative Retinopathy: Small areas of balloon-like swelling in the retina's tiny blood vessels, known as microaneurysms, occur at this earliest stage.
- Moderate Nonproliferative Retinopathy: Blood vessels that nourish the retina may swell and distort as the disease progresses. They may also lose their ability to transport blood.
- Severe Nonproliferative Retinopathy: Many more blood vessels are blocked, depriving several areas of the retina of their blood supply. These areas of the retina send signals to the body to grow new blood vessels for nourishment.
- Proliferative Diabetic Retinopathy (PDR): At this advanced stage, signals sent by the retina for nourishment trigger the growth of new blood vessels. These new blood vessels are abnormal and fragile. They grow along the retina and vitreous, the clear, jelly-like substance that fills the center of the eye. If they leak blood, severe vision loss and even blindness can result.
Risk Factors for Diabetic Retinopathy
- Duration of diabetes: The longer you have diabetes, the greater your risk of diabetic retinopathy.
- Poor blood sugar control: Keeping your blood sugar level within a range decreases the risk of diabetic retinopathy.
- High blood pressure: High blood pressure can exacerbate damage to the retinal blood vessels, increasing the risk of serious complications.
- Tobacco use: Smoking increases your risk of various diabetes complications, including diabetic retinopathy.
- High cholesterol: High levels of blood lipids can increase the risk of retinal vessel occlusion, leading to retinopathy.
Preventing Diabetic Retinopathy
Preventive measures for diabetic retinopathy focus on regular monitoring and control of your diabetes. Here are some key strategies:
- Manage your diabetes: Use your diabetes management plan as a road map. Adjust your healthy eating, physical activity, and medication plan based on your blood sugar test results.
- Keep your blood pressure and cholesterol under control: Eating a healthy diet, exercising regularly and taking your prescribed medications can help.
- Quit smoking or using other types of tobacco: Smoking increases your risk of various diabetes complications, including diabetic retinopathy.
- Pay attention to vision changes: Contact your eye doctor immediately if you experience sudden vision changes or your vision becomes blurry, spotty, or hazy.
- Get a comprehensive dilated eye exam at least once a year: Early detection and treatment can limit the potential for significant vision loss from diabetic retinopathy.
Treatment Options for Diabetic Retinopathy
Treatment for diabetic retinopathy is often delayed until it progresses to a more severe stage. Some treatment options include:
- Focal laser treatment: Also known as photocoagulation, this laser treatment can stop or slow the leakage of blood and fluid in the eye.
- Scatter laser treatment: Also known as panretinal photocoagulation, scatter laser treatment shrinks abnormal blood vessels.
- Vitrectomy: This procedure involves removing blood from the middle of the eye (vitreous) and any scar tissue tugging on the retina.
- Injections: Injecting medicine into the eye may stop new blood vessels from forming and decrease fluid buildup in the retina.
Frequently Asked Questions
-
What is the first sign of diabetic retinopathy?
- The first signs can be subtle and unnoticed without an eye exam. Early signs might include floaters, blurriness, dark areas of vision, and difficulty perceiving colors.
-
How often should I get an eye exam if I have diabetes?
- The American Diabetes Association recommends that adults with type 1 diabetes get a comprehensive eye exam within five years of their diagnosis and annually thereafter. Those with type 2 diabetes should have an exam shortly after the diagnosis and annually after that.
-
Can diabetic retinopathy be reversed?
- While early diabetic retinopathy can't be reversed, treatment can stop the progression and decrease the risk of blindness.
-
Is diabetic retinopathy only found in older adults?
- No, diabetic retinopathy can occur at any age. However, the risk increases the longer you have diabetes.
-
What are the best ways to manage diabetic retinopathy?
- The best ways to manage diabetic retinopathy involve controlling your diabetes, blood pressure, and cholesterol, along with regular eye exams.
-
Can diet and exercise influence diabetic retinopathy?
- Yes, diet and exercise play critical roles in managing diabetes, which can, in turn, impact the progression of diabetic retinopathy.
-
What is the difference between proliferative and nonproliferative diabetic retinopathy?
- Nonproliferative diabetic retinopathy is in its early stage, with mild or nonexistent symptoms. Proliferative diabetic retinopathy is in its more advanced stage, where new blood vessels begin to grow on the retina and can lead to serious vision issues.
-
Are there any new treatments for diabetic retinopathy?
- Yes, research is ongoing, and treatments are continually evolving, including newer pharmacological options targeting different disease processes.
-
Can pregnancy affect diabetic retinopathy?
- Pregnancy can exacerbate diabetic retinopathy, so pregnant women with diabetes should be monitored closely.
-
How does diabetic retinopathy affect vision over time?
- Without management, diabetic retinopathy can cause significant vision loss and even blindness over time.
Conclusion and Take-Home Message
Diabetic retinopathy is a severe health condition that requires immediate attention and ongoing management. Regular eye exams, good blood sugar and blood pressure control, and early intervention are crucial to prevent serious complications, including blindness. Empower yourself with knowledge and be proactive in your health management to maintain good eye health and overall well-being.
Bibliography
- American Diabetes Association. "Standards of Medical Care in Diabetes—2024."
- National Institutes of Health. "Diabetic Retinopathy: Hope through Research."
- Mayo Clinic. "Diabetic retinopathy."
- The Lancet. "Recent advances in understanding and managing diabetic retinopathy."
- New England Journal of Medicine. "Therapeutic Approaches to Diabetic Retinopathy."
Remember, maintaining optimal blood sugar levels and regular eye check-ups are your best defense against diabetic retinopathy. Stay informed, stay prepared, and take charge of your diabetes and eye health.
BOOK AN APPOINTMENT
It takes less than 5 minutes to complete your online booking. Alternatively, you may call our BGC Clinic, or our Alabang Clinic for assistance.