Infantile Esotropia
It is an inward deviation of one or both eyes presenting during the first six months of life in an otherwise neurologically normal child. It is sometimes called congenital esotropia, but the deviation is rarely present at birth. Although many theories exist, the true cause of infantile esotropia remains unknown.
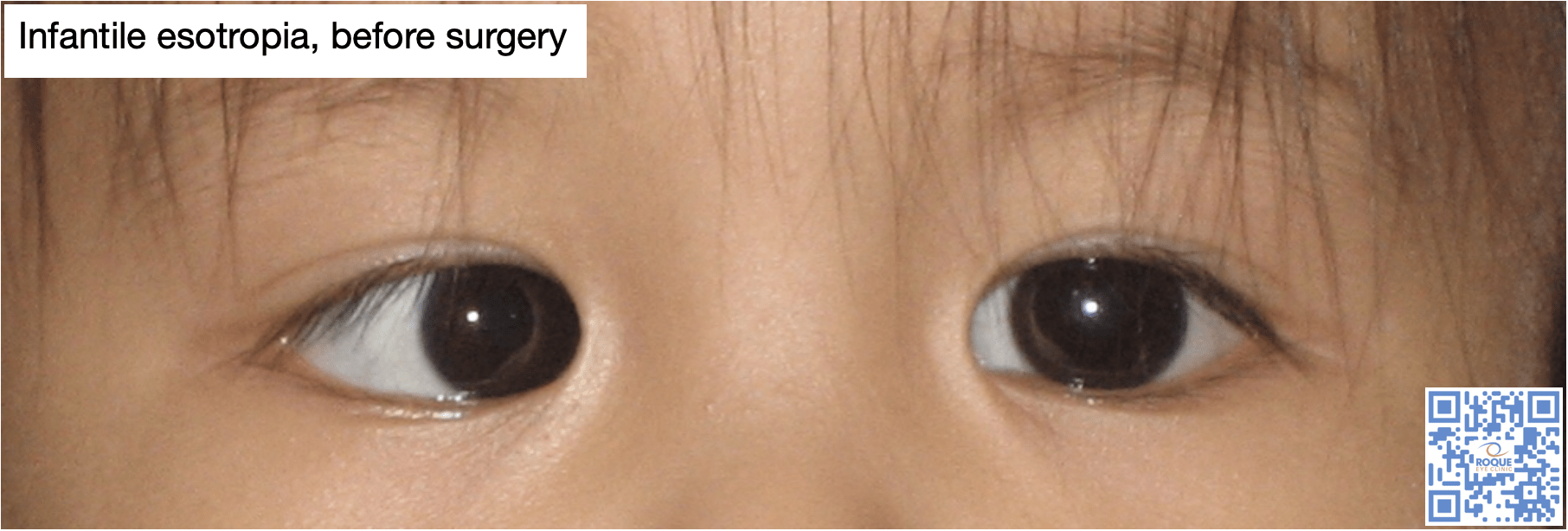
The eye deviation is known to be large and constant and affected children sometimes cross fixate to cope with it. They usually have small amounts of hyperopia and prescribing glasses does not alter the deviation.
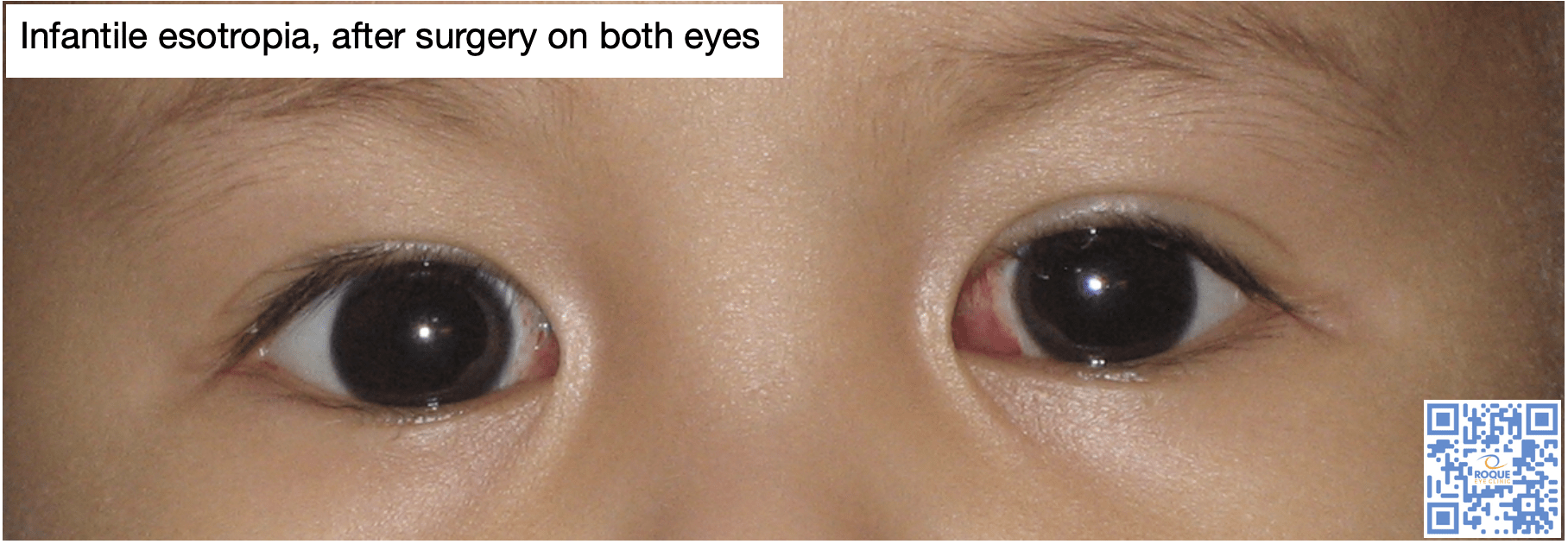
Affected children should be seen early by a pediatric ophthalmologist so that a comprehensive eye exam can be done. Glasses for hyperopia may be given but surgery should be done during infancy. Doing surgery between 1-2 years of age was found to be associated with better motor and sensory outcomes. Doing the surgery after age 3 and those with very large deviations are associated with the need for a second surgery.
Bilateral medial rectus recession is preferred over unilateral recess-resect due to better outcomes. However, despite a successful early surgery, these children could still develop other eye deviations, such as inferior oblique overaction or dissociated vertical deviation up to 2 years after surgery.
Botox injection to the eye muscles is an alternative to surgery, and may even be used as an adjunct to it for very large deviations, but it is not considered superior to it.
- Bachar Zipori, A., Spierer, O., Sherwin, J., and Kowal, L. (2020). Why bilateral medial recession fails? Factors associated with early repeated surgery. Int Ophthalmol, 40(1); 59-66.
- Hug, D. (2015). Management of infantile esotropia. Curr Opin Ophthalmol, 26(5): 371-374.
- Issaho, D., Carvalho, F., Tabuse, M., Carrijo-Carvalho, L., and de Freitas, D. (2017). The use of botulinum toxin to treat infantile esotropia: a systematic review with meta-analysis. Invest Ophthalmol Vis Sci, 58(12): 5468-5476.
- Kim, E., and Choi, D. (2019). Comparison of surgical outcomes between bimedial rectus recession and unilateral recess-resect for infantile esotropia. Ophthalmic Epidemiol, 26(2): 102-108.
- Lee, H., Kim, J., Kim, S., and Yu, Y. (2018). Relation between preoperative hyperopia and surgical outcome in infantile esotropia. Int J Ophthalmol, 11(12): 1963-1967.
- Magli, A., Rombetto, L., Matarazzo, F., and Carelli, R. (2016). Infantile esotropia: risk factors associated with reoperation. Clin Ophthalmol, 10: 2079-2083.
- Speeg-Schatz, C., Burgun, P., and Gottenkiene, S. (2017). To what extent may botulinum toxin type A injections can be an alternative choice to surgery in infantile esotropia? Eu J Ophthalmol, 27(3): 285-288.
- Wan, M., Chiu, H., Shah, A., and Hunter, D. (2018). Long-term surgical outcomes for large-angle infantile esotropia. Am J Ophthalmol, 189: 155-159.
- Wan, M., Gilbert, A., Kazlas, M., Wu, C., Mantagos, I., Hunter, D., and Shah, A. (2018). The effect of botulinum toxin augmentation to strabismus surgery for large-angle infantile esotropia. Am J Ophthalmol, 189: 160-165.
- Yabas Kiziloglu, O., Ziylan, S., and SImsek, I. (2020). Long-term motor and sensory outcome after surgery for infantile esotropia and risk factors for residual and consecutive deviations. Semin Ophthalmol, 35(1): 27-32.
- Yagasaki, T., Yokoyama, Y., and Tsukui, M. (2020). Relationship between stereopsis outcome and timing of surgical alignment in infantile esotropia. J AAPOS.