AMBLYOPIA FAQ
FAQ
Amblyopia is poor vision in one eye that cannot be attributed to any structural defect of any of its parts. It commonly affects one eye but may sometimes involve both eyes. It is caused by any abnormal visual experience very early in life, such as uncorrected refractive errors, eye misalignment (strabismus), or visual deprivation. These causes should be addressed as soon as detected. Depending on the severity, amblyopia may be reversible if the underlying causes are identified and if treatment is started early. Affected children usually do not complain of any symptom, so vision screening in preverbal or preschool children is important.
The child’s pediatrician can detect abnormal light reflexes or any apparent eye misalignments. Toddlers should be able to cooperate with some form of visual acuity testing, usually a type of picture card, or the E game. When suspicion is high, the pediatrician refers the child to a pediatric ophthalmologist to perform more specific eye examinations. Early detection is critical to the treatment of amblyopia.
After a comprehensive eye examination, it is important for the pediatric ophthalmologist to plan a course of management, depending on the clinical findings.
The more serious scenario is when there is visual deprivation in one eye, such as when a lens opacity (cataract) prevents light from passing through the eye. This requires urgent surgical excision because of its profound effect on vision if left untreated for a considerable amount of time. The promptness of surgery will eventually impact the results of postoperative amblyopia treatment. A delay in surgical removal carries a poor visual prognosis, despite intensive amblyopia treatment.
In the subset of patients who present with clear visual axes but are found to have significant refractive errors, the pediatric ophthalmologist needs to prescribe the full strength of the glasses to ensure a clear retinal image in both eyes. Approximately 30% of children with amblyopia improve with glasses alone, so a patient is usually given 2-3 months to adapt to the glasses (refractive adaptation) prior to starting amblyopia treatment.
When ocular dominance is present, it is corrected by patching or penalizing the dominant (better) eye. Patching the good eye forces the brain to use the amblyopic (non-dominant) eye to stimulate visual development. Part-time occlusion is recommended for very young children, especially those under 1 year of age, to prevent the development of occlusion amblyopia on the good eye. The earlier the intervention, the better the visual prognosis. Penalization with atropine drops is an alternative option for children who are not compliant with patching.
The success of amblyopia treatment declines with increasing age, therefore its detection is pivotal and its management should begin soon, while the visual system is still sensitive to treatment.
The Pediatric Eye Disease Investigator Group (PEDIG) is a big group of university-based and community-based pediatric ophthalmologists in the United States that studied different amblyopia treatment modalities since the early 2000s. The Amblyopia Treatment Studies is a series of randomized controlled trials comparing the effectiveness of different amblyopia treatment modalities in children with different severities of amblyopia.
The results of the studies showed that weekend atropine is as effective as 2-hour patching in moderate and severe amblyopia in children less than 7 years old. The effect of either treatment was maintained even years after termination and both seems to be effective even in some children older than 7.
The PEDIG studies also showed that 2-hour patching of the good eye is as effective as 6-hours patching in moderate amblyopia. Furthermore, they showed that 6-hour patching of the good eye is as effective as full-time patching in severe cases.
With the guidance of the pediatric ophthalmologist, parents and patients have the option to choose the best-tolerated treatment method. The course of treatment may take 6-12 months and compliance is the key to successful treatment. In general, a very good response is appreciated in patients younger than 7 years old, but a decline in effect starts to show at age 5 years old. Nevertheless, it is still worth trying in older children. A yearly follow-up is suggested once amblyopia has been successfully treated to monitor for regression.
In cases of amblyopia due to unequal refractive errors, compliance with glasses and conventional amblyopia treatment may be very challenging. Refractive surgical modalities, like laser surgery, phakic intraocular lenses implantation, and refractive lens exchange can be unique means to reduce the refractive error in selected patients. Although their risk profiles are higher than that of traditional therapies, they offer an opportunity for improving visual acuity in children who otherwise would have poor visual outcomes traditional amblyopia treatment.
- Donahue, S., Arthur, B., Neely, D., Arnold, R., Silbert, D., Ruben, J., POS Vision Screening Committee. (2013). Guidelines for automated preschool vision screening: a 10 year, evidence-based update. J AAPOS, 17(1): 4-8.
- Holmes, J., Kraker, R., Beck, R., Birch, E., Cotter, S., Everett, D., Hertle, R., Quinn, G., Repka, M., Scheiman, M., Wallace, D., Pediatric Eye Disease Investigator Group (2003). A randomized trial of prescribed patching regimens for treatment of severe amblyopia in children. Ophthalmology, 110(11): 2075-2087.
- Holmes, J., Lazar, E., Melia, B., Astle, W., Dagi, L., Donhaue, S., Frazier, M., Hertle, R., Repka, M., Quin, G., Weise, K., Pediatric Eye Disease Investigator Group (2011). Effect of age on response to amblyopia treatment in children. Arch Ophthalmol, 129(11): 1451-1457.
- Kraus, C., and Culican, S. (2018). New advances in amblyopia therapy II: refractive therapies. Br J Ophthalmol, 102(12): 1611-1614.
- Pediatric Eye Disease Investigator Group (2002). A randomized trial of atropine versus patching for treatment of moderate amblyopia in children. Arch Ophthalmol, 120(3): 268-278.
- Pediatric Eye Disease Investigator Group (2008). A randomized trial of near versus distance activities while patching for amblyopia in children aged 3 to less than 7 years. Ophthalmology, 115(11): 271-278.
- Pediatric Eye Disease Investigator Group, Repka, M., Kraker, R., Beck, R., Holmes, J., Cotter, S., Birch, E., Astle, W., Chandler, D., Felius, J., Arnold, R., Tien, D., Glaser, S. (2008). A randomized trial of atropine versus patching for treatment of moderate amblyopia: follow-up at age 10 years. Arch Ophthalmol, 126(8): 1039-1044.
- Repka, M., Beck, R., Holmes, J., Birch, E., Chandler, D., Cotter, S., Hertle, R., Kraker, R., Moke, P., Quinn G., Scheiman, M., Pediatric Eye Disease Investigator Group (2003). A randomized trial of patching regimens for treatment of moderate amblyopia in children. Arch Ophthalmol, 121(5): 603-611.
- Repka, M., Cotter, S., Beck, R., Kraker, R., Birch, E., Everett, D., Hertle, R., Holmes, J., Quin, G., Sala, N., Scheiman, M., Stager, D. Sr., Wallace, D., Pediatric Eye Disease Investigator Group (2004). A randomized trial of atropine regimens for treatment of moderate amblyopia in children. Ophthalmology, 111(11): 2076-2085.
- Repka, M., Kraker, R., Beck, R., Birch, E., Cotter, S., Holmes, J., Hertle, R., Hoover, D., Klimek, D., Marsh-Tootle, W., Scheiman, M., Suh, D., Weakley, D., Pediatric Eye Disease Investigator Group (2009). Treatment of severe amblyopia with weekend atropine: results from 2 randomized clinical trials. J AAPOS, 13(3): 258-263.
- Repka, M., Kraker, R., Holmes, J., Summers, A., Glaser, S., Barnhardt, C., Tien, D.; Pediatric Eye Disease Investigator Group (2014). Atropine versus patching for the treatment of moderate amblyopia: follow-up at 15 years of age of a randomized clinical trial. JAMA Ophthalmol, 132(7): 799-805.
- Repka, M., Wallace, D., Beck, R., Kraker, R., Birch, E., Cotter, S., Donahue, S., Everett, D., Hertle, R., Holmes, J., Quin, G., Scheiman, M., Weakley, D., Pediatric Eye Disease Investigator Group (2005). Two-year follow-up of a 6-month randomized trial of atropine versus patching for treatment of moderate amblyopia in children. Arch Ophthalmol, 123(2): 149-157.
- Scheiman, M., Hertle, R., Kraker, R., Beck, R., Birch, E., Felius, J., Holmes, J., Kundart, J., Morrison, D., Repka, M., Tamkins, S.; Pediatric Eye Disease Investigator Group (2008). Patching versus atropine to treat amblyopia in children aged 7-12 years: a randomized trial. Arch Ophthalmol, 126(12): 1634-1642.
- Scheiman, M, Hertle, R., Beck, R., Edwards, A., Birch, E., Cotter, S., Crouch, E. Jr., Cruz, O., Davitt, B., Donahue, S., Holmes, J., Lyon, D., Repka, M., Sala, N., Silbert, D., Suh, D., Tamkins, S., Pediatric Eye Disease Investigator Group (2005). Randomized trial treatment of amblyopia in children aged 7-17 years. Arch Ophthalmol, 123(4): 437-447.
- Wallace, D., Pediatric Eye Disease Investigator Group, Edwards, A, Cotter, S., Beck, R., Arnold, R., Astle, W., Barnhardt, C., Birch, E., Donahue, S., Everett, D., Felius, J., olmes, J., Kraker, R., Melia, M., Repka, M., Sala, N., Silbert, D., Weise, K. (2006). A randomized trial to evaluate 2 hours of daily patching for strabismic and anisometropic amblyopia in children. Ophthalmology, 113(6): 904-912.
AMBLYOPIA VIDEO
BOOK AN APPOINTMENT
It takes less than 5 minutes to complete your online booking. Alternatively, you may call our BGC Clinic, or our Alabang Clinic for assistance.
OUR AMBLYOPIA SPECIALIST
DR. BARBARA ROQUE
MD, DPBO, FPAO, FPCS
Dr. Barbara Roque is a specialist in pediatric ophthalmology, adult strabismus, and ophthalmic genetics. Her private practice began in 2006, after her post-graduate fellowship training at The Children’s Hospital in Westmead, University of Sydney System, Australia. Her patients are mostly children with ocular disease, refractive errors, cataracts, and eye misalignment.
OUR CLINICS
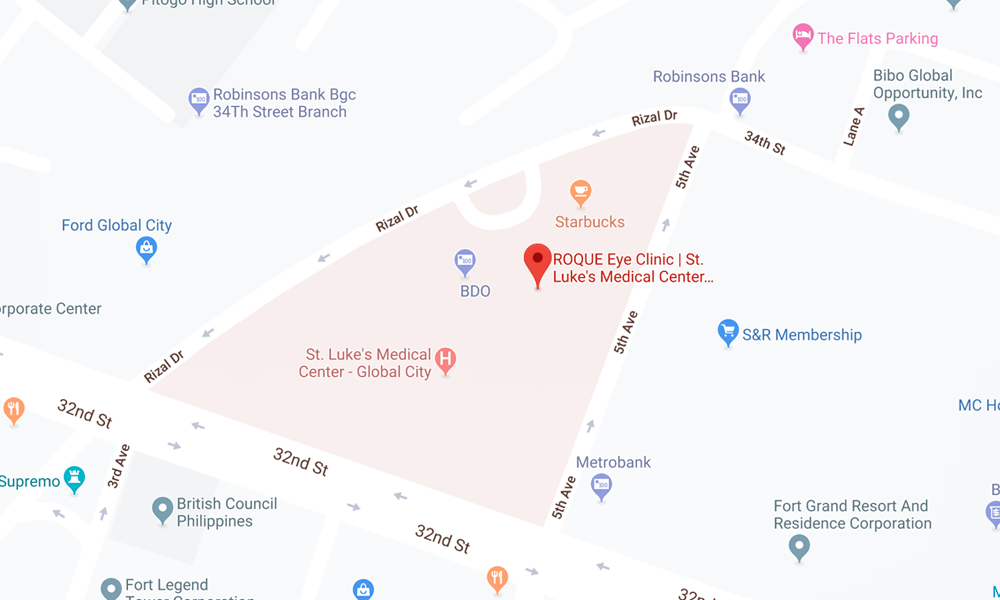
BGC CLINIC
- ST. LUKE'S MEDICAL CENTER GLOBAL CITY
2/F Medical Arts Building 217
Rizal Drive corner 5th Avenue
Bonifacio Global City, Taguig 1634
Philippines
SLMC CLINIC HOURS
- 9am - 12pm
Appointments only
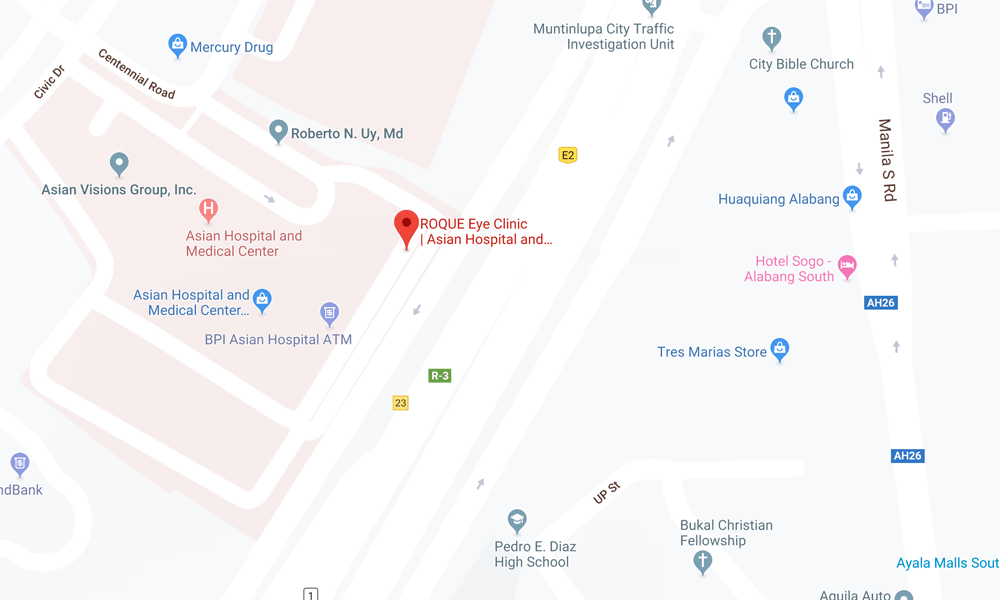
ALABANG CLINIC
- ASIAN HOSPITAL AND MEDICAL CENTER
5/F Medical Office Building 509
2205 Civic Drive, Filinvest City
Alabang, Muntinlupa 1781
Philippines
AHMC CLINIC HOURS
- 1pm - 4pm
Appointments only
BOOK AN APPOINTMENT
It takes less than 5 minutes to complete your online booking. Alternatively, you may call our BGC Clinic, or our Alabang Clinic for assistance.