You are here because you have been searching for answers to cataract questions.
These may include its definition, cataract symptoms, surgery (phacoemulsification, FLACS), intraocular lens implant options, cataract surgery packages, and other frequently asked questions.
We have all the answers for you, including videos, animations, and comparison tables.
CATARACT QUICK LINKS
- Section 1 - What is a cataract
- Section 2 - What to do when you have a cataract
- Section 3 - Estimated timeline
- Section 4 - Cataract surgery
- Section 5 - eMedicine Feature article
- Section 6 - Intraocular lens implant options
- Section 7 - Cataract surgery fees
- Section 8 - Post-operative care
- Section 9 - Frequently asked questions
WHAT IS A CATARACT?
The most common age-related eye disease affecting vision is a cataract. Surgery to remove cataracts is one of the most frequently performed, successful, and safest medical procedures today. If you or your loved one would like to get rid of eyeglasses or improve the quality of sight, then cataract surgery may be the solution.
Animation & Video
WHAT TO DO WHEN YOU HAVE A CATARACT
Videos
By adding videos and animations, we have made it easy for you to learn about cataract surgery. There are also tables comparing numerous intraocular lenses and packages.
Book your cataract evaluation via Online Booking. Alternatively, you may call up our BGC Clinic or our Alabang Clinic to speak with one of our staff.
Tests
Our staff will assist you with booking your refractive cataract surgery diagnostic examinations at the eye center. Depending on your ocular status, you may also need to have the following done: keratograph, fundus photo, OCT, B-scan, etc.
Counseling
The ophthalmic diagnostic test results will be evaluated by Dr. Manolette Roque during your clinic visit. The best surgical approach and intraocular lens implant will be offered based on your vision requirements, ocular status, and budget.
Scheduling
Once you have decided on your cataract surgery, picked your intraocular lens, and have the necessary HMO letter of authorization (LOA), Philhealth pre-approval, and retina/medical clearance, you may pick the nearest available surgical slot, at your convenience.
ESTIMATED TIMELINE
PLANNED SURGERY DAY MINUS 7 TO 90 DAYSAt least 1 week prior to surgery
EXAMINATION & COUNSELING
Ocular examination is performed in clinic. This may include, but is not limited to, refraction, slit-lamp biomicroscopy, ocular surface examination, ophthalmic pressure checks, and dilated fundus examination. Once eye diagnostic results are available, intraocular lens implant computation may be made, and the power is chosen. This power is unique to your eyes and is ordered from the distributors. If they are available in stock, they may be delivered within a day or two. If they are unavailable, shipping from the manufacturer may take 1-2 weeks. If the lens needs to be customized, it may be fully prepaid and ordered. Customized lenses may take 6-12 weeks to make and deliver.
EYE DIAGNOSTICS
Cataract screening tests (refraction, biometry, specular microscopy, topography, dry eye keratograph, retina fundus photos, OCT, etc.) are performed at the eye center/institute. The results are generally valid for around 90 days. We prefer to repeat the tests for cataract surgeries performed after 3 months from the date of examination.
LABORATORY EXAMINATIONS
Blood extraction, ECG, and x-ray, if necessary, are requested and performed at the laboratory. If they are not within normal limits, then a medical clearance will be requested. Laboratory results are usually accepted for review within one to two weeks from extraction/imaging.
MEDICAL CLEARANCE
Laboratory results are taken to the internist for cardiopulmonary clearance. Blood sugar and blood pressures are commonly silently elevated in our subset of patients. If you do not have a current internal medicine doctor, we can refer you to one.
INSURANCE GOP
Insurance companies issue a guarantee of payment (GOP) several days prior to the surgery date. The validity is variable. If your insurance has coverage for an intraocular lens (IOL) implant, a separate GOP for IOL coverage must be secured.
PHILHEALTH PRE-APPROVAL
Philhealth requires a minimum of 5 business days to process cataract surgery pre-approval. Our staff will assist you in securing this.
PLANNED SURGERY DAY MINUS 3 DAYSThree days prior to surgery
HMO LOA
Each Health Maintenance Organization (HMO) issues a letter of authorization (LOA) with a short validity of 3 days only. It is, therefore, important to finalize your surgical schedule before requesting an LOA from your HMO. A separate LOA for IOL coverage must be secured if your HMO has coverage for an intraocular lens (IOL) implant.
COVID RT-PCR NASAL SWAB
Most cataract surgeries are performed under local anesthesia. Patients who have completed their COVID-19 vaccinations and booster shots are no longer required to present a COVID-19 negative RT-PCR. Unvaccinated patients must present a negative COVID-19 RT-PCR nasal swab performed three days before surgery. Currently, hospitals have not yet recognized COVID RT-PCR saliva tests as a suitable alternative.
PLANNED SURGERY DAY 0Cataract Surgery Day
OUT PATIENT, DAY SURGERY
This is the day you have been preparing for. The actual day to say goodbye to your cloudy vision. The surgery is usually performed under topical (eye drop) anesthesia. Sometimes, cases are performed under monitored anesthesia care or light sedation. Less commonly, it is performed under general anesthesia. Cataract surgery is usually completed within half an hour, from start to finish. You will spend more time getting yourself admitted and prepared for surgery and awaiting billing and discharge from the hospital.
POST-OPERATIVE EXAMINATION
After the surgery, you will be asked to begin your eye drops while awaiting final discharge. Once discharged, you will be asked to proceed to the clinic for an immediate post-op examination before your departure to your residence. Alternatively, an immediate same-day post-operative examination may be scheduled 1-2 days after the surgery.
OPHTHALMIC MEDICATIONS
Our main job is over. It is your turn to follow the prescribed ophthalmic medications. Our clinic will give you written and digital prescriptions. These eye drops are meant to minimize intraocular inflammation and prevent potential infection, providing you with the best visual outcomes.
POST-OPERATIVE DAY 2 ONWARDSAt least two days post-op
CATARACT SURGERY ON THE OTHER EYE
Surgery on the fellow eye is usually performed at least two days after surgery of the initial eye. The schedule is variable. Most of our patients prefer to have them done a couple of days apart to have only one period of 'down time' applying ophthalmic medications. Some patients prefer to have the other eye done once the initial eye has healed completely.
POST-OPERATIVE WEEK 1-2One to two weeks post-op
ROUTINE POST-OP VISIT
Your eye will be examined. The intervals of application of ophthalmic medications will be revised. This is your intermediate eye check up.
POST-OPERATIVE WEEK 5-6Four to six weeks post-op
ROUTINE POST-OP VISIT
You will have very little ophthalmic medications left at this time. You may be given ophthalmic lubricants and oral supplements.
POST-OPERATIVE MONTH 3-6Three to six months post-op
FINAL REFRACTION, ETC.
A final refraction and specular microscopy are performed at this time. If you feel that you need post-operative prescription glasses to further improve the quality of your vision, then you may purchase a new pair of prescription glasses.
POST-OPERATIVE YEAR 1-2One to two years post-op
SECONDARY CATARACT, POSTERIOR CAPSULE OPACIFICATION
Secondary opacification of the posterior capsule, which wraps around the artificial intraocular lens implant, may lead to 'cloudy' or blurred vision. This is not a true cataract but a result of the healing process. This may be removed with a single out-patient procedure called YAG laser capsulotomy. Vision quality improves immediately after the procedure.
ANNUAL WELL EYE EXAMINATION
An annual eye examination is recommended to screen for aging eye conditions, and maintain ocular health.
CATARACT SURGERY
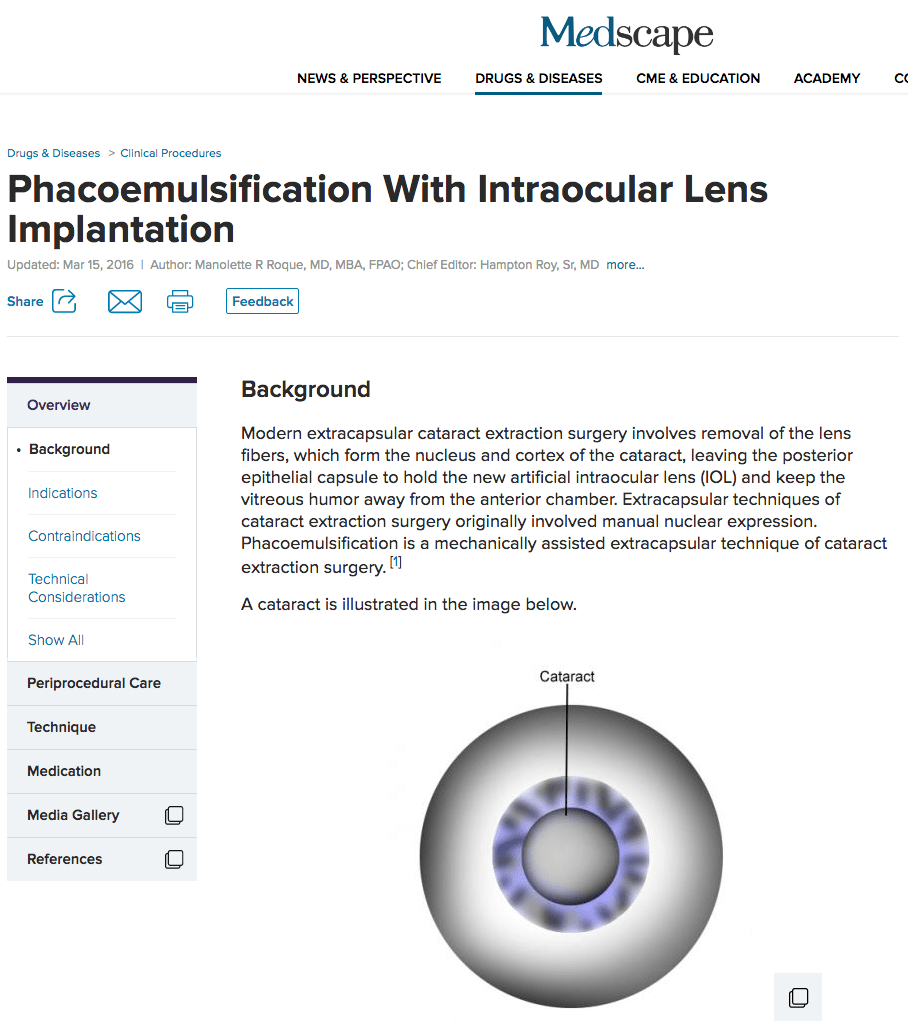
Phacoemulsification
Phacoemulsification is a machine-assisted cataract surgery technique allowing small sutureless corneal incisions with foldable intraocular lens implantations. Click on the eMedicine link below to read up on a manuscript on phacoemulsification which Dr. Roque prepared for eMedicine Medscape.
FLACS
A small instrument will be placed between your eyelids to keep you from blinking. In Bladeless Laser Cataract Surgery (aka Femtosecond Laser-Assisted Cataract Surgery or FLACS), the laser is used to make the opening in the eye, an opening in the lens itself, and to treat the lens. Dr. Roque uses the advanced Alcon LenSx system. If needed, an ultrasonic instrument will then gently break the cataract into microscopic particles, which are then suctioned away.
PHACOEMULSIFICATION FEATURE
eMedicine Medscape Ophthalmology
Phacoemulsification with Intraocular Lens Implantation
Authored by Dr. Manolette Roque for eMedicine Medscape Ophthalmology
INTRAOCULAR LENS IMPLANT OPTIONS
An appropriate intraocular lens (IOL) for your specific visual requirements has been chosen preoperatively.
This IOL may be an
- ASPHERIC MONOFOCAL (Alcon Clareon Monofocal AutonoMe, Alcon IQ, Freedom Focus, Hoya iSert 250, Hoya iSert 251, HumanOptics Aspira, J&J Tecnis, J&J Tecnis Eyhance, Medicontur Bi-Flex T, Ocuflex, Ophtec Precizon, PhysIOL microAY123, Rayner Aspheric, VSY Acriva, and Zeiss CT Asphina),
- ASPHERIC MONOFOCAL TORIC (Alcon Clareon Toric (soon), Alcon IQ Toric, HumanOptics Toric A, J&J Tecnis Eyhance Toric II, J&J Tecnis Toric II, Medicontur Toric, Ophtec Precizon Toric, Rayner Toric, and Zeiss TORBI),
- (EDOF) EXTENDED DEPTH OF FOCUS (Alcon Clareon Vivity (soon), Alcon IQ Vivity, J&J Tecnis Symfony, Teleon Lentis Comfort)
- (EDOF) EXTENDED DEPTH OF FOCUS TORIC (Alcon Clareon Vivity Toric (soon), Alcon IQ Vivity Toric, J&J Tecnis Symfony Toric II, Teleon Lentis Comfort Toric)
- ASPHERIC MULTIFOCAL (Alcon Clareon Panoptix (soon), Alcon IQ Panoptix, HumanOptics Diffractiva, HumanOptics Triva, Medicontur Liberty, Ophtec Precizon Presbyopic, PhysIOL FineVision microF, Rayner Trifocal, Teleon Lentis MplusX, VSY RevIOL, Zeiss AT Lisa, and Zeiss AT Lisa Tri),
- ASPHERIC MULTIFOCAL TORIC (Alcon Clareon Panoptix Toric (soon), Alcon IQ Panoptix Toric, HumanOptics ToricaDiff, Medicontur Liberty Toric, PhysIOL PodFT, Rayner Trifocal Toric, Teleon Lentis MplusX Toric, and Zeiss AT Lisa Toric)
The IOL you chose to correct your vision is inserted into your natural lens's exact location. Once the IOL is locked into position, the micro-incision seals itself, typically without the need for sutures. It remains tightly closed by the outward pressure within the eye and provides fast and much more comfortable recovery.
IOL Options
- IOL Comparison Table
- Video | IOL Options
- Animation | IOL Options
- Toric
- Enhanced Monofocal
- EDoF
- Zeiss EDoF
- Diffractive
- Refractive
- Zeiss Trifocal
- Segmented
- Accommodative
- Piggyback
- Scleral-Fixated
| MONOFOCAL | MONOFOCAL TORIC | MULTIFOCAL | MULTIFOCAL TORIC | EDOF VARIFOCAL POLYFOCAL | ADD ON | |
|---|---|---|---|---|---|---|
| Distance Vision | Yes | Yes | Yes | Yes | Yes | Yes |
| Intermediate Vision | No | No | Yes | Yes | Yes | Yes (Multifocal only) |
| Near Vision | No | No | Yes | Yes | Yes | Yes (Multifocal only) |
| Astigmatism Correction | No | Yes | No | Yes | Yes (Varifocal Toric only) | Yes (Toric only) |
| Aspheric | Yes | Yes | Yes | Yes | Yes | Yes |
| Preloaded | Yes (Hoya 251, Micro123, Aspira, Bi-Flex HL) | No | Yes (AT LISA Tri) | No | No | No |
| Brands | Alcon Clareon Monofocal AutonoMe, Alcon IQ, Freedom Focus, Hoya iSert 250, Hoya iSert 251, HumanOptics Aspira, J&J Tecnis, J&J Tecnis Eyhance, Medicontur Bi-Flex T, Ocuflex, Ophtec Precizon, PhysIOL microAY123, Rayner Aspheric, VSY Acriva, and Zeiss CT Asphina | Alcon Clareon Toric (soon), Alcon IQ Toric, HumanOptics Toric A, J&J Tecnis Eyhance Toric II, J&J Tecnis Toric II, Medicontur Toric, Ophtec Precizon Toric, Rayner Toric, and Zeiss TORBI | Alcon Clareon Panoptix (soon), Alcon IQ Panoptix, HumanOptics Diffractiva, HumanOptics Triva, Medicontur Liberty, Ophtec Precizon Presbyopic, PhysIOL FineVision microF, Rayner Trifocal, Teleon Lentis MplusX, VSY RevIOL, Zeiss AT Lisa, and Zeiss AT Lisa Tri | Alcon Clareon Panoptix Toric (soon), Alcon IQ Panoptix Toric, HumanOptics ToricaDiff, Medicontur Liberty Toric, PhysIOL PodFT, Rayner Trifocal Toric, Teleon Lentis MplusX Toric, and Zeiss AT Lisa Toric | Alcon Clareon Vivity (soon), Alcon Clareon Vivity Toric (soon), Alcon IQ Vivity, Alcon IQ Vivity Toric, J&J Tecnis Symfony, J&J Tecnis Symfony Toric II, Teleon Lentis Comfort, Teleon Lentis Comfort Toric, Teleon Lentis MPlus MF20, Teleon Lentis MPlusX, Teleon Lentis MPlusX Toric, Teleon Lentis MPlus MF30, WIOL | Toric, Multifocal, SML |
CATARACT SURGERY | PHACOEMULSIFICATION
CATARACT SURGERY
| SENIOR CITIZEN & PWD | NON-SENIOR-CITIZEN & NON-PWD | |||||||
|---|---|---|---|---|---|---|---|---|
| PROFESSIONAL FEE (PER EYE) | ||||||||
| YES | NO | YES | NO | PHILHEALTH | YES | NO | YES | NO |
| YES | YES | NO | NO | HMO/INSURANCE | YES | YES | NO | NO |
| 0 | 6,400 | 30,000 | 35,715 | CASH OUT-OF-POCKET | 0 | 6,400 | 43,600 | 50,000 |
| ONE INTRAOCULAR LENS (IOL) IMPLANT | ||||||||
| 71,430 | PREMIUM IOL | 100,000 | ||||||
| 32,143 | STANDARD IOL | 45,000 | ||||||
| 10,000 | BASIC IOL | 14,000 | ||||||
| Third party payors (HMO/Insurance) or the patient pays for the hospital fees. | HOSPITAL FEES | Third party payors (HMO/Insurance) or the patient pays for the hospital fees. | ||||||
LEGEND
- IOL. Intraocular Lens implant. Implanted to improve vision after cataract surgery.
- PHILHEALTH. Philippine Health Insurance Corporation. First Payor. If cataract surgery is pre-approved, Philhealth provides coverage of 16,000 pesos. 9,600 pesos is retained by the hospital. 6,400 is released to the surgeon.
- HMO. Health Maintenance Organization. Second Payor. Provides coverage, after Philhealth, for the rest of the hospital bill and professional fees. If Philhealth is not available, the HMO usually requires the individual to shoulder the Philhealth coverage of 16,000 pesos. An IOL is usually not covered and is paid out of pocket.
- BASIC. Cataract surgery is performed to remove the opacified crystalline lens and decrease refractive error. A monofocal intraocular lens (IOL) that corrects a single point of focus, usually far is implanted. It provides clear distance vision, but does not correct astigmatism and near vision. The individual must use progressives or bifocals.
- STANDARD. Cataract surgery is performed to remove the opacified crystalline lens and decrease refractive error. Astigmatism is removed with a Toric IOL implant or limbal relaxing incisions. Astigmatism is a type of refractive error in which the eye does not focus light evenly on the retina, resulting in distorted or blurred vision at all distances. Computer (intermediate) and reading (near) glasses are required.
- PREMIUM. Cataract surgery is performed to remove the opacified crystalline lens and decrease refractive error. A multifocal or Extended Depth of Focus (EDOF) IOL that corrects all distances (far, intermediate, near) is implanted. Premium IOLs provide around 90% spectacle independence in the real-world setting. One may need to use prescription glasses 10% of the time (small print, low light conditions, bright light conditions). MULTIFOCAL lenses are less dependent on reading glasses, but have more glare and halos at night. EDOF lenses require +1.00 to +1.25 D for near vision tasks, but have less glare and halos.
- PRESBYOPIA. Presbyopia is a condition associated with age. As people age, the lens becomes harder and less elastic, making it more difficult for the eye to focus on close objects. Presbyopia correcting IOLs, e.g., multifocal IOLs, correct all distances. See MULTIFOCAL.
- ADDON. A second intraocular lens implant is inserted in an anatomic space called the sulcus in front of an existing intraocular lens placed in the capsular bag. It may correct for post-operative spherical refractive errors, astigmatism, and presbyopia. The SML, Scharioth Macula Lens, is a Low Vision implant useful for patients with age-related macular degeneration or another maculopathy (central vision problems).
- NON-ASPHERIC (SPHERICAL). A spherical intraocular lens can induce minor optical imperfections called higher-order aberrations (HOAs), which can affect the quality of vision, particularly in low-light conditions such as driving at night.
- ASPHERIC. Premium aspheric IOLs approximate the shape and optical quality of the eye's natural lens and provide sharper vision, especially in low light conditions and for people with large pupils.
- Cataract Surgery with intraocular lens implantation under local anesthesia is performed:
- by Dr. Manolette Roque
- in St. Luke's Medical Center Global City each Monday, Wednesday, and Friday afternoon. Scheduled patients must arrive one (1) hour before surgery. If cataract surgery is under general anesthesia, patients must arrive two (2) hours before surgery.
- in Asian Hospital Medical Center, in Alabang, Muntinlupa every Tuesday, and Thursday morning. Scheduled patients must arrive two (2) hours prior to surgery.
- with any of the following phacoemulsification units: Zeiss Quatera 700, Alcon Centurion, Alcon Infiniti, or B+L Stellaris.
- with the Alcon LenSx Femtosecond laser for FLACS.
- Cataract screening and post-operative follow up examinations may be done in Asian Hospital MOB 509 or St. Luke's Medical Center Global City MAB 217.
- Phacoemulsification Cataract Surgery is usually performed under local anesthesia in either hospital. FLACS is only done in St. Luke’s Global City.
- STOP the following medications, one (1) week prior to planned cataract surgery:
- All blood thinners (Aspirin, Aspilet, Clopidogrel, Heparin, Enoxaparin, Ardeparin, Danaparoid, Warfarin, Vitamin E, Gingko Biloba)
- All prostate medications (Harnal, Tamsulosin, Flomax, Hytrin, Avodart, Duodart, Proscar, among others)
- The hospital fees estimate for routine cataract surgery performed under local anesthesia is around 35,000 pesos.
- If conscious sedation is requested, expect an additional 45,000 pesos or more to your hospital and anesthesiologist fees.
- If general anesthesia is required, expect an additional 80,000 pesos or more to your hospital and anesthesiologist fees.
- If the LenSx Femtosecond laser is used for FLACS, expect an additional 45,000 pesos to your hospital fees.
- Cataract surgery combined with trauma, glaucoma, uveitis, cornea, or retina diseases are much longer, require more consumables, and are therefore associated with additional expenses.
- Cataract Surgery Inclusions:
- 3 free post-operative follow-up visits (usually on day 0 or 1, week 1, month 1).
- Cataract Surgery Exclusions:
- Pre-operative consultation
- pre-operative diagnostic tests
- pre-operative medications.
- post-operative follow-up visits beyond the third visit or one month.
- YAG laser posterior capsulotomy
- Phacoemulsification Menu is inclusive of Philhealth and Senior Citizen discount whenever applicable. Senior Citizen ID and PWD ID must be shown and the official receipt must be signed to avail of the eVAT exemption. Government-mandated discounts may not be combined with other promos. Double discounting is not allowed.
- Additional charges will be billed for the use of Iris Hooks, Capsule Hooks, Malyugin Rings, IRing pupil expanders, JetRing CTR, Triamcinolone Acetonide, Anti-VEGF injections, Ozurdex Dexamethasone implant, and other devices.
- Philhealth pre-approval is required five (5) working days before the scheduled surgery. Please submit your Philhealth ID, MDR, and other documents one week before a scheduled surgery.
- Only Philippine FDA-registered IOLs may be used when availing of Philhealth benefits. For premium IOLs that are not yet registered, Philhealth may not be filed.
- HMO letter of authorization (LOA) or Insurance guarantee of payment (GOP) needs to be requested three (3) days before a scheduled surgery.
- Cancellation and No Show Policy
POST-OPERATIVE CARE
Post-operative Care
You will be released soon after the procedure to go home and relax for the rest of the day. Your eye will not be patched, and most patients can see well after surgery. Visual recovery varies from patient to patient, but most patients return to normal activities within a day or two. If you have cataracts in both eyes, the second procedure will usually be scheduled within a week or two.
Wear your protective eye goggles/shield at night, when napping, or when outdoors for 4 weeks. If you are sensitive to bright light, wear protective sunglasses. Your old glasses cannot harm your eye. If they make your vision blurry, temporary replacement lenses may be made at any time.
RESTRICTIONS FOR 4 WEEKS: DO NOT RUB YOUR EYE. (avoid direct pressure on the operated eye). NO WATER SPORTS. NO CONTACT SPORTS. NO SWIMMING. You may bathe, and/or shower. NO DIRECT SPRAY TO THE FACE. You may resume strenuous activities, and wear eye makeup after 4 weeks. You may resume your normal activities: reading, watching TV, doing household activities, etc. There are no food restrictions. If you experience any sudden and dramatic new symptoms, you should see Dr. Manolette Roque in (St. Luke's Medical Center Global City MAB 217 | Asian Hospital MOB 509) clinic immediately. Such symptoms are: (a) intense pain, especially if accompanied by nausea, light sensitivity, and heavy tearing, (b) sudden onset of new or increased number of "floaters" (spots or lines in the field of vision), (c) flashes of light in your peripheral vision, resembling lightning or the flickering of lights, (d) a curtain or dark area covering any portion of your visual field, (e) decrease in vision. You may proceed to the St. Luke's Medical Center Global City Emergency Room, after clinic hours. The ophthalmology hospitalist or ER physician will examine you, contact and, update Dr. Manolette Roque.
DILATION. Your eyes will remain dilated for approximately 8 hours after surgery. Your vision will be blurred at this time. Once the pupil returns to normal the following day, vision should improve.
HEALING. You may experience generally foggy (painless) vision for 1-7 days. Visual acuity improves to its maximum potential within 1-4 weeks. Healing is variable between individuals. DOWNTIME. You may return to work within 2-3 days after surgery, depending on how fast your vision improves.
STEROID-INDUCED GLAUCOMA. Some individuals may experience intraocular pressure (IOP) spikes secondary to the use of corticosteroids. High IOP may cause headaches and blurring of vision. Additional pressure-lowering medications may be given to control or prevent IOP spikes. These may include Brinzolamide, Timolol, Brimonidine, and Tafluprost ophthalmic solutions.
NEUROADAPTATION. Some premium multifocal lens implant users may experience haloes and glare at night, decreased contrast sensitivity, and poor vision in low-light, warm and yellow light conditions. These symptoms will decrease in intensity over time due to neuroadaptation (brain adjustment).
RESIDUAL REFRACTION. All the pre-operative examinations performed prior to cataract surgery resulted in a best-effort GUESS-TIMATE. There may be residual refractive errors that may require spectacle correction or laser enhancement surgery. These may be done 3 months after cataract surgery. These additional procedures are not included in the initial payments made and are out-of-pocket expenses.
AFTER-CATARACT. In less than 5% of cases after cataract surgery, a secondary blurring of vision may occur after 3 months to 2 years. This may be as high as 50% in individuals who choose to have multifocal IOL implants. The secondary blurring of vision is not a true cataract. It is the formation of scar tissue. Some people will get it. Others won't. The posterior capsular opacification AKA "After Cataract" may be removed with a minor office procedure called YAG laser capsulotomy. Vision will immediately return to normal, the following day. This does not recur. After your initial same-day examination, please return to see Dr. Roque in the clinic for your post-operative examination after 1 week, and 1 month.
YAG LASER POSTERIOR CAPSULOTOMY A posterior capsulotomy is a laser procedure that sometimes is necessary after cataract surgery. During cataract surgery, part of the front (anterior) capsule of the eye’s natural lens is removed to gain access to and remove the lens. The clear, back (posterior) capsule remains intact and supports an intraocular lens (IOL), a plastic or silicone disc that is implanted in the eye and replaces the natural lens. As long as that capsule stays clear, you will experience good vision. But in 30% of routine cases, the posterior capsule loses its clarity. When this happens, the ophthalmologist (Eye M.D.) can create an opening in the capsule using a laser in order to restore normal vision. This procedure is called a posterior capsulotomy. Before the laser procedure, the ophthalmologist does a thorough ophthalmic examination to make sure there is no other reason for vision loss. The posterior capsulotomy is painless and takes approximately five minutes. Eye pressure is measured 30 minutes after the operation to make sure it is not elevated, and anti-inflammatory medicated eyedrops are usually prescribed for three days following the procedure. Vision usually improves within hours. Potential but rare complications following laser posterior capsulotomy are increased intraocular pressure and retinal detachment.
Serious complications are infrequent, but there are some risks involved. One of our counselors will provide you with additional information about the risks associated with cataract surgery. Choosing an experienced surgeon for your procedure can significantly minimize the risks involved with your cataract procedure.
FREQUENTLY ASKED QUESTIONS
Frequently Asked Questions on Cataract
A cataract is a progressive clouding of the eye's natural lens that hampers light passing through the retina, causing vision problems. The most common type is related to aging. More than half of people age 65 or older have a cataract. People who suffer from cataracts usually describe the condition as similar to looking through the mist, smoke, a cloud, a waterfall, or a piece of wax paper, with a gradual blurring or dimming of vision. In the early stages, stronger lighting and eyeglasses may lessen vision problems caused by cataracts. However, surgery may be needed to improve vision at a certain point. Today, cataract surgery is safe and very effective
The lens is the part of the eye that helps focus light on the retina. The retina is the eye's light-sensitive layer that sends visual signals to the brain. Light passes through the lens and gets focused on the retina in a normal eye. To help produce a sharp image, the lens must remain clear.
More than half of people over 60, and quite a few younger than that, suffer from cataracts. It is said that everyone will develop a cataract if they live long enough.
Reading may become more difficult, and driving a car can become dangerous. Cataract sufferers may also be troubled by a bothersome glare, halos around lights, or even double vision. And as the cataract becomes worse, frequent changes in eyeglass prescriptions may become necessary.
- Age-related cataract: Most cataracts are related to aging.
- Congenital cataract: Some babies are born with cataracts or develop them in childhood, often in both eyes. These cataracts may not affect vision. If they do, they may need to be removed.
- Secondary cataract: Cataracts are more likely to develop in people who have certain other health problems, such as diabetes. Also, cataracts are sometimes linked to steroid use.
- Traumatic cataract: Cataracts can develop soon after an eye injury, or years later.
Currently, there is no medical treatment to reverse or prevent the development of cataracts. Once they form, there is only one way to achieve clear vision again, and that is to physically remove the cataract from the eye.
Although we don't know how to protect against cataracts, people over 60 are at risk for many vision problems. If you are 60 or older, you should have an eye examination through dilated pupils at least every two years. This kind of exam allows your eye care professional to check for signs of age-related macular degeneration, glaucoma, cataracts, and other vision disorders.
For an early cataract, vision may improve by using different eyeglasses, magnifying lenses, or stronger lighting. If these measures don't help, surgery is the only effective treatment. This treatment involves removing and replacing the cloudy lens with a substitute lens.
A cataract needs to be removed only when vision loss interferes with your everyday activities, such as driving, reading, or watching TV. You and your eye care professional can make that decision together. In most cases, waiting until you are ready to have cataract surgery will not harm your eye. If you decide on surgery, your eye care professional may refer you to a cataract surgeon to remove the cataract. If you have cataracts in both eyes, you may have them removed separately or simultaneously, depending on your requirements and condition.
Sometimes, a cataract should be removed even if it doesn't cause problems with your vision. For example, a cataract should be removed if it prevents examination or treatment of another eye problem, such as age-related macular degeneration or diabetic retinopathy.
Cataract removal is one of the most common operations performed in the world today. It is also one of the safest and most effective. In about 90 percent of cases, people who have cataract surgery have better vision afterward.
There are two primary ways to remove a cataract. Your doctor can explain the differences and help determine which is best for you:
Phacoemulsification, or phaco. Phacoemulsification is an advanced technique of cataract extraction. It is also known as small-incision cataract surgery. Others call it the "no-needle, no-stitch" technique. After applying a local anesthetic, your doctor makes a small incision on the side of the cornea, the clear, dome-shaped surface covering the front of the eye. The doctor then inserts a tiny probe into the eye. This device emits ultrasound waves that soften and break up the cloudy center of the lens so it can be removed by suction. Most cataract surgery today is done by phaco.
Extracapsular surgery. Your doctor makes a slightly longer incision on the cornea's side and removes the lens's hard center. The remainder of the lens is then removed by suction.
After placing topical anesthesia, clear corneal incision is made with a crystal/diamond keratome. This is usually only 2.75 mm in size. This is a self-sealing incision that allows a sutureless procedure.
Arguably, one of the more delicate steps in the procedure of cataract removal, continuous curvilinear capsulorhexis (CCC), is the careful creation of a well-controlled tear in the anterior capsule of the cataract.
Ultrasonic vibrations (phacoemulsification) are now created to crush the cataract into manageable particles, which are then aspirated into a port using the same tip (handpiece).
The conventional way of approaching the removal of a cataract is by the "divide and conquer" method. The cataract is rotated, and grooving is continued to create manageable pie-shaped segments.
This provides a side view of the actual inclination of the phaco tip (handpiece) as it proceeds with phacoemulsification of the cataract.
After removal of the tough nuclear component, the softer cortical material is then aspirated with an irrigation/aspiration (I/A) handpiece. Complete cataract removal lessens the likelihood of developing an "after-cataract" or posterior capsular opacification necessitating a YAG laser capsulotomy post-operatively.
After injection of viscoelastic material into the capsular bag and the anterior chamber, a foldable intraocular lens is then inserted and unfolded into the eye.
The intraocular lens is then dialed into place. The remaining viscoelastic material is removed. The eye is then checked for leaks.
In most cataract surgeries, the removed lens is replaced by an intraocular lens (IOL). An IOL is a clear, artificial lens that requires no care and becomes a permanent part of your eye. With an IOL, you'll have improved vision because light can pass through it to the retina. Also, you won't feel or see the new lens. The self-sealing corneal incision precludes the need for stitches. However, one may receive one or several stitches in some instances.
Some people cannot have an IOL. They may have problems during surgery, or maybe they have another eye disease. For these people, a soft contact lens may be suggested. For others, glasses that provide powerful magnification may be better.
A week or two before surgery, your eye care professional will do some tests. These may include tests to measure the cornea's curvature and the size and shape of the eye. For patients who will receive an IOL, this information helps your doctor choose the right type of IOL. Also, doctors may ask you not to eat or drink anything after midnight the morning of your surgery.
When you enter the hospital or clinic, you will be given eye drops to dilate the pupil. The area around your eye will be washed and cleansed.
The operation usually lasts less than 1 hour and is almost painless. Many people choose to stay awake during surgery, while others may need to be put to sleep for a short time. If you are awake, you will have an anesthetic to numb the nerves in and around your eye.
After the operation, a patch will be placed over your eye, and you will rest for a while. Your medical team will watch you see if there are any problems, such as bleeding. Most people who have cataract surgery can go home the same day. Since you will not be able to drive, make arrangements for a ride.
It's normal to feel itching and mild discomfort for a while after cataract surgery. Some fluid discharge is common, and your eye may be sensitive to light and touch. If you have discomfort, your eye care professional may suggest a pain reliever every 4-6 hours. After 1-2 days, even moderate discomfort should disappear. In most cases, healing will take about six weeks.
After surgery, your doctor will schedule exams to check on your progress. You may take eye drops or pills for a few days after surgery to promote healing and control the pressure inside your eye. Ask your doctor how to use your medications, when to take them, and what effects they can have. You will also need to wear an eye shield or eyeglasses to help protect the eye. Avoid rubbing or pressing on your eye.
Problems after surgery are rare, but they can occur. These can include infection, bleeding, inflammation (pain, redness, swelling), vision loss, or light flashes. With prompt medical attention, these problems can usually be treated successfully.
Try not to bend or lift heavy objects when you are home. Bending increases pressure in the eye. You can walk, climb stairs, and do light household chores.
You can quickly return to many everyday activities, but your vision may be blurry. The healing eye needs time to adjust to focus properly with the other eye, especially if the other eye has a cataract. Ask your doctor when you can resume driving.
If you just received an IOL, you may notice that colors are very bright or have a blue tinge. Also, if you've been in bright sunlight, everything may be reddish for a few hours. If you see these color tinges, it is because your lens is clear and no longer cloudy. Within a few months after receiving an IOL, these colors should disappear. And when you have healed, you may enjoy your enhanced vision.
If you chose a monofocal IOL, you would always need reading glasses. If you chose a multifocal IOL, you would be able to read without eyeglasses, provided you have adequate lighting conditions. Astigmatism correcting IOLs decreases your requirement for prescription glasses after cataract surgery.
Sometimes, a part of the natural lens that is not removed during cataract surgery becomes cloudy and may blur your vision. This is called an after-cataract. An after-cataract can develop months or years later. Unlike a cataract, an after-cataract is treated with a laser. With YAG laser capsulotomy, your doctor uses a laser beam to make a tiny hole in the lens to let light pass through. This is a painless outpatient procedure.
BOOK AN APPOINTMENT
It takes less than 5 minutes to complete your online booking. Alternatively, you may call our BGC Clinic, or our Alabang Clinic for assistance.