Capillary Hemangioma
Capillary hemangioma or “strawberry nevus” is the most common vascular ocular tumor in children. It is an abnormal growth of vascular tissue that is more commonly seen in females and in premature babies. There is no apparent familial inheritance pattern.
In 30% of cases, this vascular lesion is present at birth and its natural course is unique. It is usually small during the first few weeks of life, then, it progressively increases in size over the next 3-6 months. This phase is followed by a period of stabilization and a period of spontaneous regression by the age of 4-7 years. Thirty percent regress by 3 years old, 60% by 4 years, and 70% by 7 years.
Although capillary hemangioma is benign, periocular hemangioma carries the risk of deprivation amblyopia if the resultant ptosis is blocking the visual axis. Amblyopia is seen in 40-60% of orbital lesions. Moreover, bulky eyelid tumors often cause distortion of the eyeball causing corneal astigmatism. Prolonged occlusion of the visual axis may also lead to myopia, and the resultant inequality in the refractive error of the two eyes (anisometropia) may be another contributory factor in the development of amblyopia. Secondary strabismus may develop as a result of interruption of binocular vision.
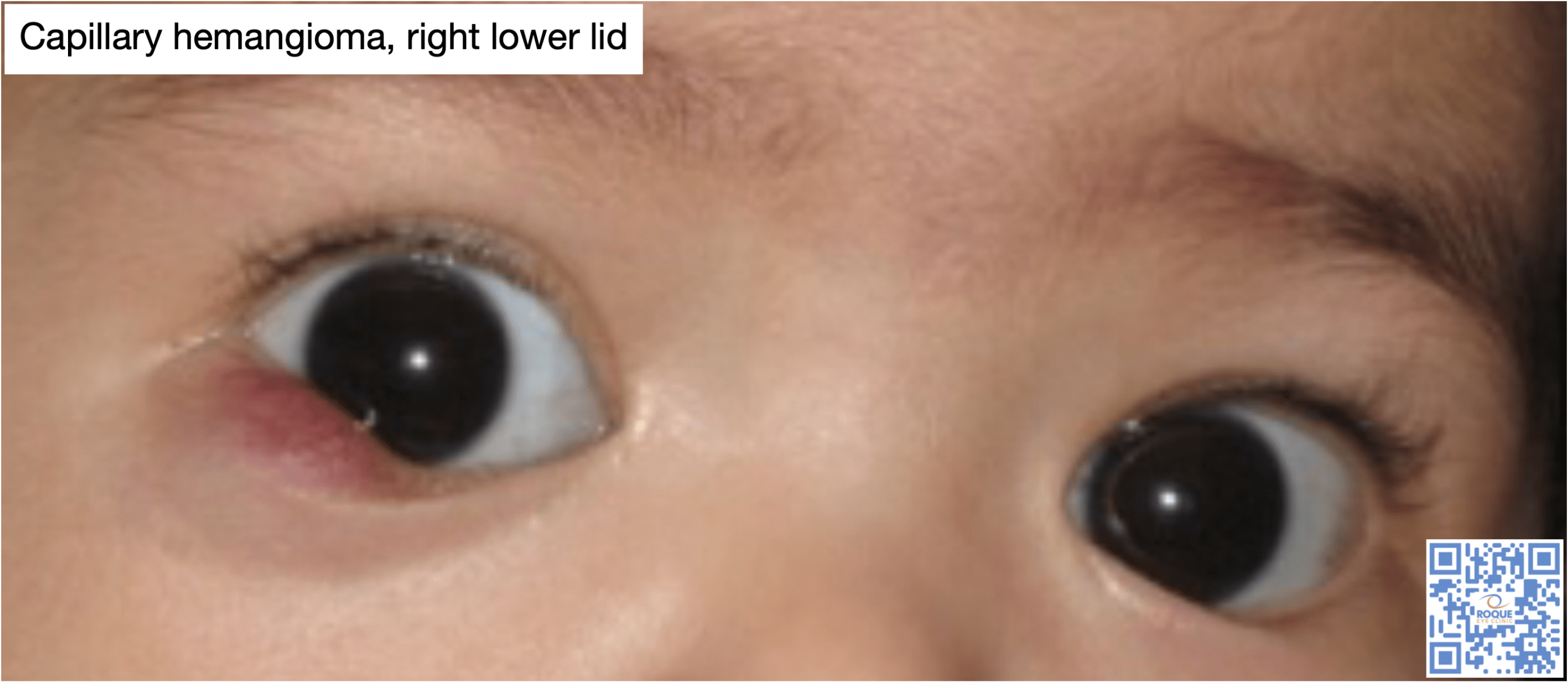
The clinical findings are often enough to reach a clinical diagnosis in majority of cases. Lesions are commonly found in the upper lid or orbit, and their appearance depend on the depth of involvement. Superficial tumors have a red lobulated strawberry appearance, which gave rise to the name “strawberry nevus”. They may increase in size or become bluish with crying. Deeper tumors appear bluish or may show no significant skin color change. The diagnosis can be facilitated by everting the eyelid to visualize the vascularity of the hemangioma. Approximately one-third of lesions are located deep in the orbit, and may present with proptosis only, without any associated skin discoloration. A helpful diagnostic sign is an increase in proptosis with crying. Occasionally the proptosis may be severe enough to cause corneal exposure. In other cases, the enormous growth may obliterate facial structures. Neuroimaging such as MRI will document the extent of the tumor.
Currently oral and topical beta-blockers like Propranolol, are the treatment of choice. The treatment could last 6-12 months. Oral and intralesional steroid have been abandoned as treatment due to side effects like hormonal imbalance, growth retardation and scarring.
Surgical excision is reserved for small localized lesions that failed to respond to oral and topical beta-blockers. It is usually avoided in larger lesions because of the risk of considerable bleeding, and because the infiltrative nature of the lesion requires removal of large amounts of skin. Laser procedures are limited by the scarring that they produce.
- Al-Haddad, C., El Salloukh, N., and El Moussawi, Z. (2019). B-blockers in the treatment of periocular infantile hemangioma. Curr Opin Ophthalmol, 30(5): 319-325.
- Chambers, C., Katowitz, W., Katowitz, J., and Binenbaum, G. (2012). A controlled study of topical 0.25% timolol maleate gel for the treatment of cutaneous infantile capillary hemgniomas. Ophthalmic Plastic Reconstr Surg, 28(2): 103-106.
- Jefferson, R., and Hildebrand, G. (2019). Topical timolol treatment for periocular infantile hemangioma in the developing world. Trop Doct, 49(3): 246-248.
- Koka, K., Mukherjee, B., and Agarkar, S. (2018). Effect of oral propranolol on periocular capillary hemangiomas of infancy. Pediatr Neonatol, 59(4): 390-396.
- Marey, H., Elmazar, H., Mandour, S., and Khairy, H. (2018). Combined oral and topical beta blockers for the treatment of early proliferative superficial periocular infantile capillary hemangioma. J Pediatr Ophthalmol Strabismus, 55(1): 37-42.
- Painter, S., and Hildebrand, G. (2016). Topical timolol maleate 0.5% solution for the management of deep periocular infantile hemangiomas. J AAPOS, 20(2): 172-174.