CATARACT FAQ
EYE Focus - Cataract FAQs
- Age-related cataract: Most cataracts are related to aging.
- Congenital cataract: Some babies are born with cataracts or develop them in childhood, often in both eyes. These cataracts may not affect vision. If they do, they may need to be removed.
- Secondary cataract: Cataracts are more likely to develop in people who have certain other health problems, such as diabetes. Also, cataracts are sometimes linked to steroid use.
- Traumatic cataract: Cataracts can develop soon after an eye injury, or years later.
Currently there is no medical treatment to reverse or prevent the development of cataracts. Once they form, there is only one way to achieve clear vision again, and that is to physically remove the cataract from the eye.
Although we don't know how to protect against cataracts, people over the age of 60 are at risk for many vision problems. If you are age 60 or older, you should have an eye examination through dilated pupils at least every 2 years. This kind of exam allows your eye care professional to check for signs of age-related macular degeneration, glaucoma, cataracts, and other vision disorders.
For an early cataract, vision may improve by using different eyeglasses, magnifying lenses, or stronger lighting. If these measures don't help, surgery is the only effective treatment. This treatment involves removing the cloudy lens and replacing it with a substitute lens.
A cataract needs to be removed only when vision loss interferes with your everyday activities, such as driving, reading, or watching TV. You and your eye care professional can make that decision together. In most cases, waiting until you are ready to have cataract surgery will not harm your eye. If you decide on surgery, your eye care professional may refer you to a specialist to remove the cataract. If you have cataracts in both eyes, the doctor will not remove them both at the same time. You will need to have each done separately.
Sometimes, a cataract should be removed even if it doesn't cause problems with your vision. For example, a cataract should be removed if it prevents examination or treatment of another eye problem, such as age-related macular degeneration or diabetic retinopathy.
There are two primary ways to remove a cataract. Your doctor can explain the differences and help determine which is best for you:
Phacoemulsification, or phaco. Phacoemulsification is an advanced technique of cataract extraction. It is also known as small-incision cataract surgery. Others call it the "no-needle, no-stitch" technique. After application of a local anesthetic, your doctor makes a small incision on the side of the cornea, the clear, dome-shaped surface that covers the front of the eye. The doctor then inserts a tiny probe into the eye. This device emits ultrasound waves that soften and break up the cloudy center of the lens so it can be removed by suction. Most cataract surgery today is done by phaco.
Extracapsular surgery. Your doctor makes a slightly longer incision on the side of the cornea and removes the hard center of the lens. The remainder of the lens is then removed by suction.
After placing topical anesthesia, clear corneal incision is made with a crystal/diamond keratome. This is usually only 2.75 mm in size. This is a self-sealing incision which allows a sutureless procedure.
Arguably one of the more delicate steps in the procedure of cataract removal, continuous curvilinear capsulorhexis (CCC) is the careful creation of a well-controlled tear in the anterior capsule of the cataract.
Ultrasonic vibrations (phacoemulsification) are now created to crush the cataract into manageable particles which are then aspirated into a port using the same tip (handpiece).
The conventional way of approaching the removal of a cataract is by the "divide and conquer" method. The cataract is rotated and grooving is continued to create manageable pie shaped segments.
This provides a side view of the actual inclination of the phaco tip (handpiece) as it proceeds with phacoemulsification of the cataract.
After removal of the tough nuclear component, the softer cortical material are then aspirated with an irrigation/aspiration (I/A) handpiece. Complete removal of the cataract lessens the likelihood of developing an "after cataract" or posterior capsular opacification necessitating a YAG laser capsulotomy post operatively.
After injection of viscoelastic material into the capsular bag and the anterior chamber a foldable intraocular lens is then inserted and unfolded into the eye.
The intraocular lens is then dialed into place. The remaining viscoelastic material is removed. The eye is then checked for leaks.
In most cataract surgeries, the removed lens is replaced by an intraocular lens (IOL). An IOL is a clear, artificial lens that requires no care and becomes a permanent part of your eye. With an IOL, you'll have improved vision because light will be able to pass through it to the retina. Also, you won't feel or see the new lens. The self-sealing corneal incision precludes the need for stitches, however, one may receive one or several stitches in some instances.
Some people cannot have an IOL. They may have problems during surgery, or maybe they have another eye disease. For these people, a soft contact lens may be suggested. For others, glasses that provide powerful magnification may be better.
When you enter the hospital or clinic, you will be given eye drops to dilate the pupil. The area around your eye will be washed and cleansed.
The operation usually lasts less than 1 hour and is almost painless. Many people choose to stay awake during surgery, while others may need to be put to sleep for a short time. If you are awake, you will have an anesthetic to numb the nerves in and around your eye.
After the operation, a patch will be placed over your eye and you will rest for a while. You will be watched by your medical team to see if there are any problems, such as bleeding. Most people who have cataract surgery can go home the same day. Since you will not be able to drive, make sure you make arrangements for a ride.
It's normal to feel itching and mild discomfort for a while after cataract surgery. Some fluid discharge is also common, and your eye may be sensitive to light and touch. If you have discomfort, your eye care professional may suggest a pain reliever every 4-6 hours. After 1-2 days, even moderate discomfort should disappear. In most cases, healing will take about 6 weeks.
After surgery, your doctor will schedule exams to check on your progress. For a few days after surgery, you may take eyedrops or pills to help healing and control the pressure inside your eye. Ask your doctor how to use your medications, when to take them, and what effects they can have. You will also need to wear an eye shield or eyeglasses to help protect the eye. Avoid rubbing or pressing on your eye.
Problems after surgery are rare, but they can occur. These can include infection, bleeding, inflammation (pain, redness, swelling), loss of vision, or light flashes. With prompt medical attention, these problems usually can be treated successfully.
When you are home, try not to bend or lift heavy objects. Bending increases pressure in the eye. You can walk, climb stairs, and do light household chores.
You can quickly return to many everyday activities, but your vision may be blurry. The healing eye needs time to adjust so that it can focus properly with the other eye, especially if the other eye has a cataract. Ask your doctor when you can resume driving.
If you just received an IOL, you may notice that colors are very bright or have a blue tinge. Also, if you've been in bright sunlight, everything may be reddish for a few hours. If you see these color tinges, it is because your lens is clear and no longer cloudy. Within a few months after receiving an IOL, these colors should go away. And when you have healed, you will probably need new glasses.
BOOK AN APPOINTMENT
It takes less than 5 minutes to complete your online booking. Alternatively, you may call our BGC Clinic, or our Alabang Clinic for assistance.
OUR DOCTORS
DR. MANOLETTE ROQUE
MD, MBA, DPBO, FPAO, FPCS
Dr. Manolette Roque is a specialist in uveitis, cataract, and refractive surgery. His private practice began in 2000, after his post-graduate fellowship at the Massachusetts Eye and Ear Infirmary, Harvard Medical School, in Boston, Massachusetts, USA. His patients are mostly adults who desire spectacle independence. His advocacy includes taking care of individuals with ocular inflammatory diseases.
Everyone deserves the best eye care possible.
DR. BARBARA ROQUE
MD, DPBO, FPAO, FPCS
Dr. Barbara Roque is a specialist in pediatric ophthalmology, adult strabismus, and ophthalmic genetics. Her private practice began in 2006, after her post-graduate fellowship training at The Children’s Hospital in Westmead, University of Sydney System, Australia. Her patients are mostly children with ocular disease, refractive errors, cataracts, and eye misalignment.
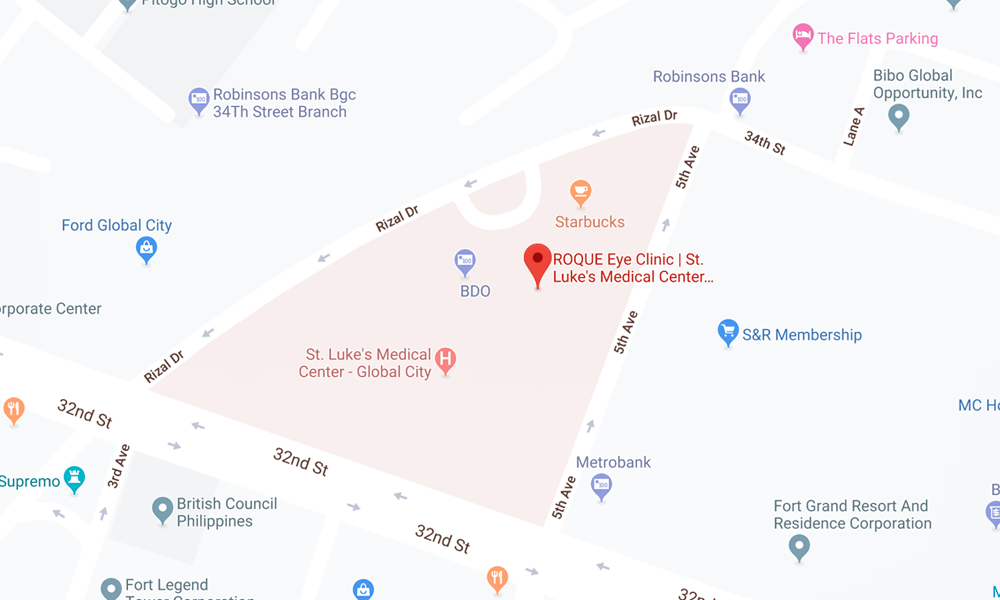
OUR CLINICS
BGC CLINIC
- ST. LUKE'S MEDICAL CENTER GLOBAL CITY
2/F Medical Arts Building 217
Rizal Drive corner 5th Avenue
Bonifacio Global City, Taguig 1634
Philippines
SLMC CLINIC HOURS
- 9am - 12pm
Appointments only
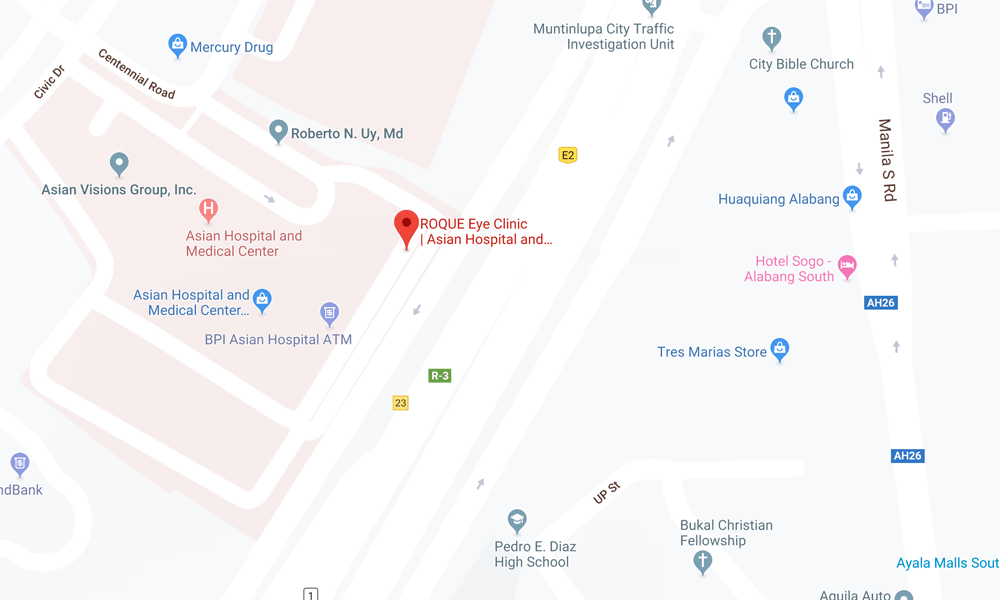
ALABANG CLINIC
- ASIAN HOSPITAL AND MEDICAL CENTER
5/F Medical Office Building 509
2205 Civic Drive, Filinvest City
Alabang, Muntinlupa 1781
Philippines
AHMC CLINIC HOURS
- 1pm - 4pm
Appointments only
BOOK AN APPOINTMENT
It takes less than 5 minutes to complete your online booking. Alternatively, you may call our BGC Clinic, or our Alabang Clinic for assistance.